Fatigue due to axial SpA (AS) can be very severe and impact on your daily life; it doesn’t feel like normal tiredness or short-term lack of sleep, it’s an overwhelming feeling of exhaustion. It can be due to the condition itself or a knock-on effect from long-term disrupted sleep. There are lots of things you can do to help reduce or manage fatigue.
What causes fatigue?
There are lots of possible causes of fatigue in axial SpA (AS), including:
- Active inflammation
- Chronic pain, particularly if it affects your ability to sleep comfortably
- Some pain medications can cause drowsiness
- Muscle weakness
- Anaemia related to inflammation
- Depression can cause physical symptoms, including fatigue
Managing axial SpA (AS)
As always, it’s really important to speak to your rheumatologist if your axial SpA (AS) is not controlled enough. Fatigue due to active inflammation is something your rheumatologist may use to decide whether to change the way you manage your condition. If your fatigue is impacting your activities or daily life, or you’re experiencing frequent flares, speak to your rheumatology team for specialist advice.
Your rheumatologist may refer you to an Occupational Therapist specialising in this area or a course to help you manage your fatigue. Fatigue is an important symptom to discuss with your rheumatologist, because there may be something they can do to help.
When to see your GP
Fatigue can also be caused by other medical conditions, such as anaemia, so it’s important to speak to your GP. Your doctor can check for any other causes of fatigue and give individualised advice.
If you’re unsure whether your pain medications are causing drowsiness or fatigue, speak to a pharmacist for a medicines review. They may be able to make suggestions such as adjusting the time of day you take your medication. If the pharmacist thinks it’s necessary, they will suggest you speak to your GP or rheumatologist about possible alternatives.
Fatigue can affect you mentally, as well as physically. If you are concerned about your mood levels or think you may have depression, speak to your GP about the range of advice and support on offer. Physical and mental health go hand in hand and one can easily impact on the other.
Pacing
Pacing is about balancing activity and rest to help learn to manage your fatigue. Although it sounds like the easiest piece of advice to follow, it’s actually very difficult. It can be very effective at managing fatigue, but it requires a good understanding of the principles of pacing, combined with commitment to making them work for you.
It’s very easy to get into a boom and bust cycle by overdoing it on a ‘good day’ and then spending days recovering afterwards. It can be very difficult, but it’s important to pace well even during good days. You may have to remind yourself about pacing more on those days, but it’s well worth it.
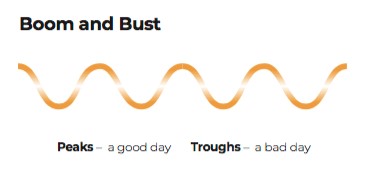
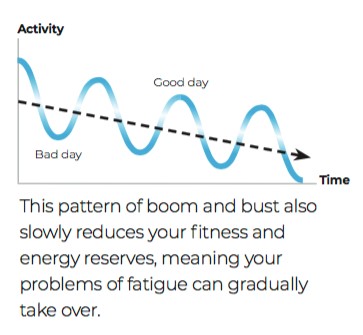
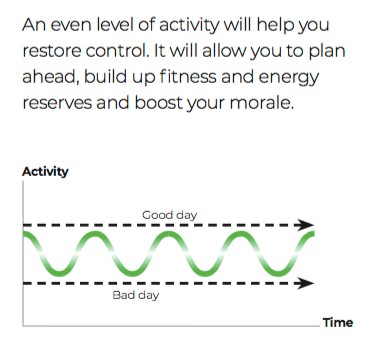
The nature of axial SpA (AS), with flares and fluctuations of symptoms, can make it very difficult to predict how much is ‘too much’. The important thing to remember is that you can always strive to pace well, but do not tell yourself off if you overdo it one day. You’re only human! Sometimes fatigue will worsen for seemingly no reason and it’s not your fault. There are some practical tips that can help with pacing.
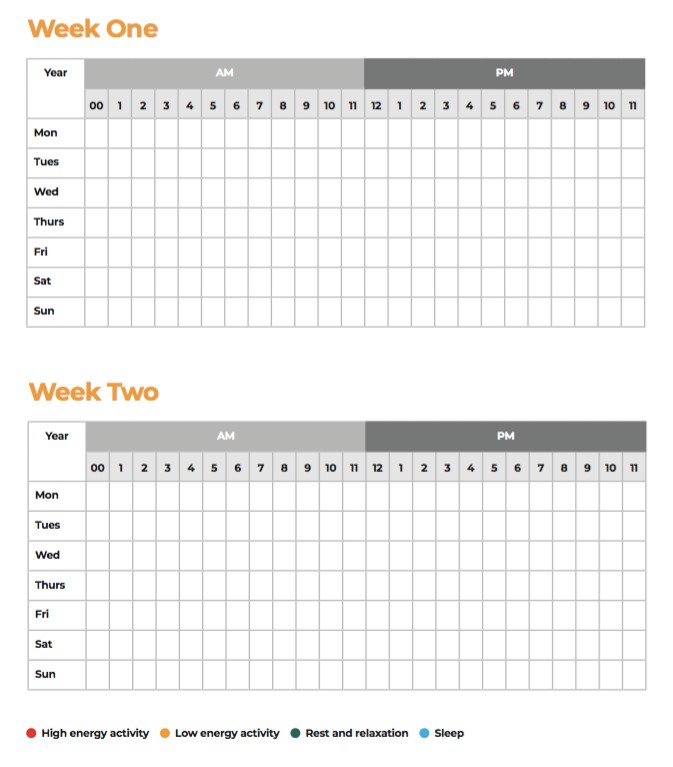
Keep a diary
Our guide “Living with axial SpA (AS) Fatigue” has a template diary to track your activities, your rest time and your sleep. It’s colour coded so you can easily look at the week and assess how you’re pacing your activities. You may then be able to suggest changes to your week to manage your fatigue.
Prioritise tasks and activities
After using the diary for a period of time, you can assess how to prioritise tasks and activities. This can be helpful because it’s sometimes difficult to know how much energy you will have in the day. If you have any important or urgent tasks, prioritise these and do them first to ensure you get them done. Then you can move onto other tasks if you have the energy afterwards.
Break tasks down into smaller jobs
Assess any task that you’re planning and, if needed, break down into smaller tasks that you can spread out over time to pace yourself.
Get a pacing buddy
If you know someone else with a condition that causes fatigue, you can be each other’s pacing buddy. The role is to give each other a friendly, non-judgmental nudge if one of you is overdoing it and at risk of aggravating fatigue.
It’s also helpful to have a buddy who you are comfortable talking to and discussing your axial SpA (AS) with. Talking about how you’re feeling can be really helpful for your mental health.
Ask for help
Speak with your friends and family to discuss how they can help you in different ways. It’s best to do this on a day when you’re feeling well, because during a higher pain or fatigue day, it may be difficult to articulate what you need.
It’s important for friends and family to understand that they can’t tell how you’re feeling based on how you look. Good communication is key, because pain and fatigue are invisible. It’s also important to explain that your needs will vary day to day.
Some people find the Spoon Theory very helpful for explaining chronic fatigue to loved ones.
Don’t be afraid to say no
When managing fatigue, there will be times you have to say no to someone for your own wellbeing. It can be very difficult, but over time this will get easier. It can be helpful to explain that sometimes you have to say no, even when you don’t want to.
Plan meals
Eating well is important to keep your energy up, so planning meals in advance will help ensure you’re prepared for high fatigue days. Bulk cook and freeze meals so that you have a back up if you’re unable to cook.
Resting
Rest doesn’t have to mean sleep, there are lots of different activities that are restful, but will keep your mind occupied. For example:
- Reading
- Watching TV
- Crafting
- Speaking to someone
- Having a warm bath
- Meditating
- Breathing exercises (link to breathing exercise sheet)
- Relaxation techniques
Rest periods can be spread throughout the day, such as resting for ten-minutes every hour or so. There is no correct way of planning your rest times, it will be very different for each person and depending on your symptoms each day.
Sleep
Pain disrupting your sleep over a long period of time can cause severe chronic fatigue. For detailed advice about managing night pain and general sleep advice, you can watch our previous video or read the blog post. (Links to night pain video and blog)
Exercise
It can seem counter-intuitive, but exercising regularly can help you manage fatigue. Breaking exercises down into smaller sessions can help reduce the tiredness you feel afterwards.
Muscle weakness can aggravate fatigue, so it’s important to do some strength training each day. Simple sit-to-stand exercises or arm exercises using light weights (or tins) are a great place to start. You can build up to doing press-ups against a wall and lunges.
Some people progress to doing exercise classes, such as yoga or Pilates. For exercise classes, it’s important to start with a beginner’s class and find an instructor who has good knowledge of your condition. Be sure to modify any exercises to ensure they are safe for you.
Exercise is really important for managing axial SpA (AS) long-term, so discuss with your rheumatologist or physiotherapist any barriers to exercise that you experience. They will be able to help you form achievable, individualised goals with a plan on how to reach them.
Diet and nutrition
There is no set diet to help with fatigue, but it’s important to maintain well-balanced nutrition. Over-eating and under-eating can cause fatigue, so it’s important to plan your meals well.
Maintaining a health weight and drinking plenty of water to prevent dehydration can improve energy levels. If you have anaemia, your GP may prescribe iron tablets, but ensuring you have lots of iron-rich foods in your diet can be a useful addition. Iron-rich foods include:
- Meat
- Beans
- Nuts
- Dried fruit
- Liver (but avoid during pregnancy)
- Wholegrains
- Cereals fortified with iron
- Most dark green leafy vegetables
If you would like to make major changes to your diet, speak to your GP or a nutritionist for specialised advice first. The NHS website has good information on vitamins and minerals.
Leave room for your golf balls
I really recommend watching Occupational Therapist Clare Clark’s video on leaving room for your golf balls.
You can watch my video on this subject here and if you have any top tips for managing fatigue that we haven’t discussed, please leave a comment.
Zoë Clark is an osteopath living with axial SpA herself and has joined the NASS Helpline team to help with the unprecedented demand over COVID-19. You may have seen her blog posts previously written for NASS and she spoke at the latest parliamentary meeting in January and appeared on Channel 5 News. She’s joining the NASS team to help you keep active and feeling well during this difficult time of isolation.
Zoë is available on the Helpline each day, so if you’d like to have a chat then please get in touch and we can arrange a call. She’ll also be sharing some of her top tips and answering any common questions, so please let us know in the comments if there’s any particular advice you’d like.
The Helpline is open 1000-1600 Monday to Friday on 020 8741 1515 or you can email zoe@nass.co.uk